Symptoms and Treatment of Heel Bone Fractures

One of the most common indicators of a fractured heel bone is tenderness in the area that causes pain, even with slight pressure. Swelling in the foot and ankle area is another prevalent symptom, often accompanied by visible bruising. Individuals with heel fractures usually find it impossible to bear weight on the affected foot, leading to significant mobility limitations. The diagnosis of heel bone fractures typically involves X-rays and computed tomography, or CT, scans. X-rays can provide a clear image of the injury, but in more complex cases, CT scans may be used to obtain a detailed, three dimensional view of the affected area. Non surgical treatment involves protecting the fractured area with a splint, resting the foot by avoiding weight-bearing, and using crutches. Once swelling subsides, a podiatrist may apply a cast to stabilize the fracture. Surgical intervention may be necessary when the fracture affects the joint. It is important to avoid putting any weight on the injured heel until the fracture has fully healed, which may take several months. If you believe you have fractured your heel bone, it is suggested that you make an appointment with a podiatrist.
Many people suffer from bouts of heel pain. For more information, contact one of our podiatrists of Sayville Foot Care. Our doctors can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in Sayville, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain
Have you ever gotten up from a chair or out of bed in the morning, and upon taking that first step, feel like your heel has stepped on a tack? Many people experience a feeling of sharp pain which radiates into their arch from their heel and which does not allow them to put their heel on the floor. Sometimes they need to sit back down, stand only on their toes and use the wall for balance. If you can take a few steps, it seems to go away and lessen, allowing you to then resume your activity. Later, throughout your day and after a period of rest, it can happen again. If this sounds familiar you may be suffering from your first attack of heel pain.
Heel pain is a debilitating condition that affects day to day activities. Running and walking both causes stress on the heel because the heel is the part of the foot that hits the ground first. This means that the heel is taking on your entire weight. Diagnosis and treatments for heel pain can be easily found through your podiatrist.
Plantar Fasciitis
One of the main causes of heel pain is a condition known as plantar fasciitis. The plantar fascia is a band of tissue that extends along the bottom of the foot, from the toe to the bottom of the heel. A rip or tear in this ligament can cause inflammation of these tissues, resulting in heel pain. People who do not wear proper fitting shoes are often at risk of developing problems such as plantar fasciitis. Unnecessary stress from ill-fitting shoes, weight change, excessive running, and wearing non-supportive shoes on hard surfaces are all causes of plantar fasciitis.
Achilles Tendonitis
Achilles tendonitis is another cause of heel pain. Similar to plantar fasciitis, inflammation of the Achilles tendon will cause heel pain due to stress fractures and muscle tearing. A lack of flexibility of the ankle and heel is an indicator of Achilles tendonitis. If left untreated, this condition can lead to plantar fasciitis and cause even more pain on your heel.
Heel Spur
A third cause of heel pain is a heel spur. A heel spur occurs when the tissues of the plantar fascia undergo a great deal of stress, leading to a separation of the ligament from the heel bone entirely. This results in a pointed fragment of bone on the ball of the foot, known as a heel spur.
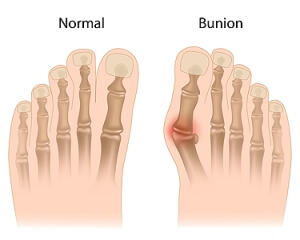
Bunion Complications
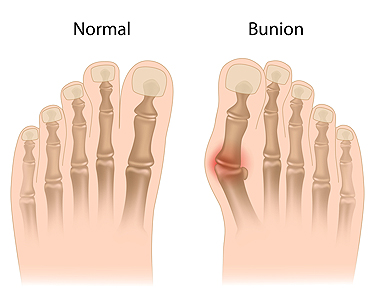
A bunion, medically termed hallux valgus, is a prominent, bony protrusion at the base of the big toe. Often, the only indicator of a mild bunion is its physical manifestation. However, it can also result in discomfort, swelling, and alterations in the foot's structure. In extreme instances, surgical intervention might be necessary due to related issues. Key visual indicators of a bunion are the big toe deviating toward the other toes, forming an outward bulge on the first foot bone. Additionally, there may be a raised bony bump on the foot's exterior, tough skin under the big toe, and calluses on the adjacent toe. Over time, the foot's form may drastically change, impacting both the big toe and other foot regions, making shoe selection challenging. Resulting structural modifications can cause pain, swelling, and bursitis, which is an inflammation of the toe joint's cushioning sac. Some people may face mobility issues with their big toe, affecting their walking. While many individuals do not encounter severe problems from bunions, if left untreated, complications such as arthritis in the big toe or deformities in the adjacent toe can arise. If you have a painful bunion, it is suggested that you make an appointment with a podiatrist who can intervene and help prevent severe complications.
If you are suffering from bunion pain, contact one of our podiatrists of Sayville Foot Care. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Sayville, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Are Bunions?
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
Seeing a Podiatrist for Cracked Heels

An individual would see a podiatrist for cracked heels because they are specialists in foot and ankle care, and cracked heels can be more than just a cosmetic issue. While minor heel fissures may be seen as a nuisance, severe cracks can be painful, bleed, or become infected. A podiatrist can identify the underlying causes of cracked heels, which may include biomechanical issues, skin conditions, systemic diseases, or prolonged pressure. This foot doctor can provide professional treatments such as debridement, where the hard, dead skin is removed safely, and prescribe specialized moisturizers or medicated creams. Additionally, they can offer guidance on footwear choices, recommend orthotic inserts to redistribute pressure, and offer advice on preventive measures. If you have persistent or severe cracked heels, it is suggested that you make an appointment with a podiatrist to ensure they are cared for and to avoid complications.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact one of our podiatrists from Sayville Foot Care. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our office located in Sayville, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
Causes, Symptoms, and Treatment of Flat Feet

Flat feet, medically known as pes planus, is a common condition where the arch of the foot is abnormally low or nonexistent, causing the entire sole to touch the ground when standing. This can be due to various factors, such as genetics, obesity, pregnancy, or repetitive high-impact activities. While some people with flat feet experience no discomfort, others may develop symptoms that affect their daily lives. Flat feet can originate in childhood, where the arch has not yet developed, and may persist into adulthood. Over time, the wear and tear on the posterior tibial tendon can lead to the arch collapsing, resulting in overpronation. Ankles and knees can also be affected, as flat feet may cause the ankles to turn inward, leading to alignment issues in the legs. Symptoms can range from difficulty standing on tiptoe to knee and back pain, arch strain, and swelling along the inside of the ankle. When it comes to treatment, a range of options can help alleviate the discomfort associated with flat feet. Special shoes with strong heel counters, steel or carbon fiber shanks, and medial postings can assist in alignment. Custom-designed arch supports, molded to your foot's unique contours, are often recommended. Stretching exercises for a shortened Achilles tendon may also prove beneficial. For help in dealing with flat feet, it is suggested that you make an appointment with a podiatrist to determine the best course of action for your specific needs.
Flatfoot is a condition many people suffer from. If you have flat feet, contact one of our podiatrists from Sayville Foot Care. Our doctors will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Sayville, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flatfoot
Flatfoot is a foot disorder that is not as straightforward as many people believe. Various types of flatfoot exist, each with their own varying deformities and symptoms. The partial or total collapse of the arch, however, is a characteristic common to all types of flatfoot. Other signs of flatfoot include:
- “Toe drift,” or the pointing outward of the toes and the front part of the foot
- The tilting outward of the heel and the tilting inward of the ankle
- The lifting of the heel off the ground earlier when walking due to a tight Achilles tendon
- Hammertoes
- Bunions
One of the most common types of flatfoot is flexible flatfoot. This variation usually starts in childhood and progresses as one ages into adulthood. Flexible flatfoot presents as a foot that is flat when standing, or weight-bearing. When not standing, the arch returns. Symptoms of flexible flatfoot include:
- Pain located in the heel, arch, ankle, or along the outside of the foot
- Overpronation, or an ankle that rolls in
- Shin splint, or pain along the shin bone
- General foot aches or fatigue
- Pain located in the lower back, hip, or knee
Your podiatrist will most likely diagnose flatfoot by examining your feet when you stand and sit. X-rays may be taken to define the severity and help determine the treatment option best for your condition. Nonsurgical treatments can include activity modification, weight loss, orthotics, immobilization, medications, physical therapy, shoe modifications, and ankle foot orthoses (AFO) devices. If nonsurgical methods prove ineffective, surgery may be considered. Multiple surgical procedures can correct flatfoot; and depending on your specific condition, one may be selected alone or combined with other techniques to ensure optimal results.
Arthritis Can Cause Pain in the Feet and Ankles
Laser Therapy and Toenail Fungus

Toenail fungus, or onychomycosis, can be stubborn and challenging to treat with traditional methods. However, recent advancements in medical technology have introduced an effective alternative, which is known as laser therapy. This innovative approach utilizes concentrated beams of light to target and eliminate the fungus residing beneath the toenail. The laser treatment process begins with the application of the laser, which penetrates the nail. This specifically targets the fungal infection while leaving the surrounding healthy tissue unharmed. The laser generates heat, effectively eradicating the fungal cells and inhibiting their ability to regrow. Laser treatment offers several advantages. It is non-invasive, requires no anesthesia, and typically involves minimal discomfort. Additionally, it can be extremely effective, often requiring fewer sessions than traditional treatments. Patients can generally resume their daily activities immediately following the procedure. As with any medical treatment, consultation with a podiatrist is crucial in determining what the best approach is for your specific condition. Laser therapy represents a promising option in the battle against stubborn toenail fungus, offering a safe, efficient, and minimally disruptive solution to restore healthy and clear nails. If you are afflicted with toenail fungus, it is suggested that you seek the counsel of a podiatrist who can determine if laser treatment is right for you.
Laser treatment can be an effective way to get rid of toenail fungus. If you have any questions about laser treatment, consult with one of our podiatrists from Sayville Foot Care. Our doctors will assess your condition and provide you with quality treatment for fungal nails.
What Are Toenail Fungal Infections?
Onychomycosis, or fungal infection of the nail, is a relatively common and non-serious condition. Around 10 percent of U.S. citizens are afflicted with fungal nails. Common forms of fungus that infect the nail include dermatophytes, yeasts, and molds.
Symptoms of Toenail Fungal Infections Include:
- Nail thickening
- Brittleness of the nail
- Discoloration of the nail
Diagnosis for Fungal Nails
Fungal infections are diagnosed by fungal culture and microscopy. This will rule out any other conditions such as nail trauma, psoriasis, lichen planus, and onychogryphosis.
What Is Laser Treatment?
Laser treatment is a non-invasive, safe, quick, and painless procedure that uses the heat from a laser to kill fungus in the nail. Each infected nail is targeted with a laser for several minutes. The treatment is usually utilized several different times over a select period. During this time, a podiatrist will keep an eye on the infection.
If you have any questions, please feel free to contact our office located in Sayville, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.