How to Choose the Right Running Shoe

Choosing the perfect pair of running shoes is essential for runners of all levels. Your choice significantly affects comfort, performance, and overall foot health. To make the right selection, start by identifying your foot type, such as neutral, pronated, or supinated. Next, consider cushioning, which should be minimal for a natural feel, maximum for long-distance shock absorption, or moderate for most runners. Shoe stability matters for injury prevention. Those with flat feet or overpronation should opt for stability features like medial posts, while high arches benefit from neutral shoes with cushioning. A proper fit is also important. Leave about a thumb's width of space between your longest toe and the shoe's front. Try on multiple pairs and take them for a test run in-store to assess comfort and stability. Also, consider the type of surface you will be running on, because road, trail, and track running require different shoe types. Running shoes can become a major investment because they should be replaced after 300-500 miles to ensure optimal performance and prevent injuries. For more help with finding the proper running shoe for your feet, it is suggested that you speak to a podiatrist.
If you are a runner, wearing the right running shoe is essential. For more information, contact one of our podiatrists from Sayville Foot Care. Our doctors can provide the care you need to keep you pain-free and on your feet.
Choosing the Right Running Shoe for Your Foot Type
To increase performance and avoid the risk of injury, it is important to choose the right running shoe based on your foot type. The general design of running shoes revolves around pronation, which is how the ankle rolls from outside to inside when the foot strikes the ground.
- Neutral runners are able to choose from a wide variety of shoes, including minimalist shoes or even going barefoot.
- Runners who overpronate, or experience an over-abundance of ankle rolling, should choose shoes that provide extra motion control and stability.
- Runners who underpronate, or supinate, have feet that have high arches and lack flexibility, preventing shock absorption. They require shoes with more flexibility and cushion.
If you have any questions please feel free to contact our office located in Sayville, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Choosing the Right Running Shoe for Your Foot Type
Running may seem like a simple to do. However, running is actually a complex movement that puts stress on the ligaments, bones, and joints of the body. Selecting the correct running shoe is important for increasing performance and avoiding risk of injury. Running shoes should be selected based on your foot type. Considerations such as trail versus road shoes are important. Your foot type dictates the degree of cushioning, stability and motion control you require. The most accurate way to learn your foot type is to visit a local shop that specializes in running shoes. Professionals can measure your arch type, stride and gait and help you with your shoe needs.
The design of running shoes is created around the idea of pronation. Pronation is the natural rolling movement of your ankle from the outside to inside when your foot strikes the ground. If you run properly you strike the ground on the outside of your heel and roll in the direction of your big toe before pushing off once more. Pronation is beneficial because it assists the lower half of your body in absorbing shock and storing energy. Those considered neutral runners pronate correctly and do not need running shoes that help correct their form. Neutral runners can choose from a wide variety of shoes, including barefoot or minimal types. However, those who have arch problems or who adopt an incorrect form while running may experience too much or too little pronation. They may require running shoes that offer additional support.
Those who overpronate experience an over-abundance of ankle rolling. Even while standing, those who severely overpronate display ankles that are angled inward. It is not uncommon for them to have flat feet or curved legs. The tendency to overpronate may cause many injuries. Areas that tend to become injured are the knees, ankles, and Achilles tendon. If you find that you have a tendency to overpronate, you should look at shoes that provide extra stability and motion-control. Motion-control shoes are straight and firm. Shoes of this type do not curve at the tip. The restricted flexibility along the middle of the shoe prohibits the foot from rolling too far inward as your foot strikes the ground.
A less common problem is underpronation. Underpronation, also called supination, is when the feet are unable to roll inward during landing. Those who underpronate have feet that lack flexibility and high arches. This prevents any kind of shock absorption, even though it does place less rotational stress on ankles and knees. This added force can cause fractures, ligament tears, and muscle strains because the legs are trying to compensate for the impact. Those who underpronate need shoes with more cushioning and flexibility. If you have a tendency to underpronate, selecting stability or motion-control shoes may cause you more problems by continuing to prevent pronation.
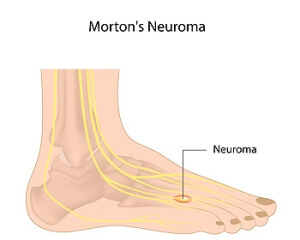
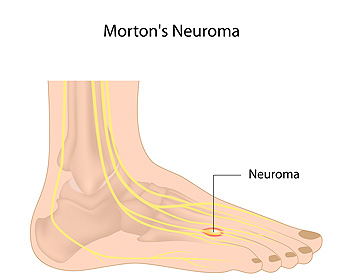
Causes and Symptoms of Morton’s Neuroma
Morton's neuroma, a painful condition affecting the feet, can develop due to a combination of factors. One primary factor is biomechanical issues within the feet, such as having flat feet or high arches. These structural variations can place excessive stress on the toe joints, leading to repeated irritation of the nerve. Tight calf muscles, which limits ankle movement, are another contributor to this condition. When the ankle's range of motion is restricted, it can result in increased pressure on the balls of the feet, further aggravating the situation. Additionally, footwear choices play a significant role in developing Morton’s neuroma. Wearing narrow, high heeled or tight fitting shoes compresses the nerves and puts pressure on the forefoot. Some patients report a persistent aching or burning sensation, frequently occurring between the third and fourth toes. This discomfort is often accompanied by sharp, shooting pains in the ball of the foot, which can extend into the toes and create additional discomfort. Some patients liken the sensation to having a foreign object such as a pebble or stone, trapped inside their shoe. Tingling and pricking sensations in the toes are also prevalent and contribute to the overall discomfort associated with Morton's neuroma. If you believe you may have Morton’s neuroma, it is suggested that you make an appointment with a podiatrist.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of Sayville Foot Care. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Sayville, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
Treatment for Plantar Warts

A plantar wart, which is a growth on the sole of your foot, is caused by exposure to the human papillomavirus, or HPV. Although this type of infection is more common among children and young adults, it can affect anyone. You might wonder how you end up with this unwelcome visitor. It's simple, the infection is caused by direct contact with the virus through a break in your skin. Sometimes, it can take months after exposure for a plantar wart to appear. The wart often starts as a small, rough patch on your foot's sole but can expand over time. These growths disrupt the usual skin lines on your feet and might display tiny black dots due to clogged blood vessels. Treatment options vary based on how the warts bother you. Salicylic acid treatments may or may not be effective. More advanced treatment includes the application of liquid nitrogen to freeze the skin, though this process can cause discomfort and may take several applications. If you think you may have a plantar wart, especially if it becomes painful or shows signs of infection, it is suggested that you make an appointment with a podiatrist. This qualified foot doctor can evaluate the problem and suggest a proper course of treatment.
Plantar warts can be very uncomfortable. If you need your feet checked, contact one of our podiatrists from Sayville Foot Care. Our doctors will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Sayville, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Warts
Plantar warts are growths that typically appear on the heels or other weight-bearing areas of the feet. These warts are caused by the human papillomavirus (HPV). The virus enters the body through breaks in the skin, such as cuts, that are on the bottom of the feet. Plantar warts are more likely to affect children and teenagers, people with weakened immune systems, people who have a history with plantar warts, and people who walk barefoot in environments exposed to a wart-causing virus.
If you suspect you have plantar warts, you may have the following symptoms: pain or tenderness while walking, a lesion that interrupts the ridges in the skin of your foot, small fleshy lesions on the bottom of the foot, or a callus where a wart has grown inward over a well-defined spot on the skin.
HPV causes plantar warts to form and is very common. There are more than 100 kinds of the virus in existence. However, only a few of them cause warts on the feet. The other types of HPV are likely to cause warts on other parts of the body.
If you have plantar warts, your podiatrist may try different treatment methods depending on your specific case. Some treatments for plantar warts are peeling medicines (salicylic acid), freezing medicines (cryotherapy), or surgical procedures. Laser treatments and vaccines are also used to treat plantar warts.
Diabetic Foot Exams

A diabetic foot exam is vital for individuals with diabetes due to their increased risk of developing foot problems resulting from nerve and blood vessel damage because of high blood sugar levels. Diabetic neuropathy, caused by this damage, can lead to numbness or a loss of sensation in the feet, making it challenging to detect calluses, blisters, or cuts. If left untreated, these issues can progress to ulcers and infections, potentially necessitating amputation. A diabetic foot exam aims to identify these problems early to prevent severe complications. The process involves gathering information about medical history, diabetes management, medications, and any symptoms experienced. A thorough skin examination checks for dryness, cracking, calluses, blisters, ulcers, or other abnormalities and compares the temperature of the feet for symmetry. Nerve function and sensation in the feet, blood flow, and foot and ankle pulses are assessed, as well as musculoskeletal problems like bent or overlapping toes. To maintain healthy feet, individuals with diabetes should perform daily self-checks and practice proper foot hygiene. If you have diabetes, it is suggested that you make an appointment to see a podiatrist and include this specialist among your healthcare providers to see regularly.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from Sayville Foot Care. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in Sayville, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Conditions
Diabetes is the condition in which the body does not properly process food for use as energy. People with Type 1 diabetes cannot produce insulin, which is required for glucose to feed your body’s cells. It is typically caused by the immune system mistaking healthy cells for foreign invaders and destroying the insulin-producing cells in the pancreas. On the other hand, people with Type 2 diabetes cannot respond to insulin properly, and eventually cannot produce enough. The Centers for Disease Control and Prevention reports that over 30 million people in the United States have diabetes, with 1 in 4 having no idea they have it. Surprisingly, diabetes is the seventh leading cause of death in the US. The symptoms of diabetes include frequent urination, fatigue, hunger, and even blurry vision.
Diabetes can also affect the feet as well. Over time, diabetes can cause nerve damage to your feet, which could then lead to symptoms such as tingling, pain and numbness in the feet. Neuropathy can be very dangerous to a person with diabetes, since it prevents them from feeling injuries such as cuts or blisters in the feet, and if not detected early enough, may lead to infection. Neuropathy can also lead changes in the shape of your feet and toes. The best way for people with diabetes to prevent or delay neuropathy is keeping their blood glucose levels in their target range. This consists of eating right, having the correct amount of exercise, and taking medications.
Diabetes can also create calluses and foot ulcers as well. Calluses build up faster and occur more frequently with those affected by diabetes. If there are too many calluses, therapeutic shoes and inserts may be required. It is important to have calluses trimmed by a health professional, as doing it yourself may lead to infections. If these calluses continue to develop and thicken, they can lead to foot ulcers. Foot ulcers are open sores, that appear on the ball of the foot or on the bottom of the big toe. These ulcers can lead to future infections if not treated and may possibly result in losing a limb. It is important to report any ulcers to your podiatrist right away. Your doctor may take x-rays to examine the foot and clean out any dead and infected tissue.
Lastly, diabetes can also lead to poor circulation and peripheral arterial disease (PAD). The poor circulation in the feet and leg area is a result of diabetes narrowing and hardening, eventually slowing down the blood flow in that area. The best way to prevent this is to keep away from smoking and follow your doctor’s advice for maintaining blood pressure and cholesterol. PAD is similar to this complication. PAD is when blood vessels narrow or are blocked by fatty deposits. PAD also increases your risk of heart attacks and strokes and is a common condition to those affected by diabetes. The combination of both PAD and neuropathy may lead to infections and can result in amputation of certain limbs. PAD can be prevented with wearing the proper foot wear and regularly taking care of your feet.
If you want to take care of your feet, you should wash and dry them carefully and perform daily inspections to check for cuts, blisters, or swelling. Any physical activity you partake in should be approved by your health care provider. You should also be sure to wear special shoes if advised to do so by your doctor.
Are Bunions Affecting Your Everyday Life?
Causes and Effective Solutions for Ankle Pain

Ankle pain can be a persistent and debilitating issue that affects individuals of all ages and lifestyles. This discomfort often stems from a variety of factors, such as injuries resulting from accidents or sports-related activities, overuse, improper footwear, or underlying medical conditions. Understanding the root cause of ankle pain is crucial for implementing effective remedies. Resting and elevating the affected foot can provide initial relief by reducing inflammation while promoting healing. Gentle stretching and strengthening exercises under the guidance of a podiatrist can aid in rehabilitation and prevent future issues. Wearing supportive footwear with proper arch and ankle support, in addition to orthotic inserts, can provide stability and alleviate pain. It is suggested that you seek timely medical advice from a podiatrist if you have ankle pain, who can effectively diagnose and treat this condition.
Ankle pain can be caused by a number of problems and may be potentially serious. If you have ankle pain, consult with one of our podiatrists from Sayville Foot Care. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendonitis
- Achilles tendon rupture
- Stress fractures
- Bursitis
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact our office located in Sayville, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.